Dear Joshua,
It’s been 5 years since you left this earth. This year you would’ve been 17, that’s sometimes really hard to wrap my mind around. You missed so much yet I remain here because of you and your parents. I imagine you would be going into your senior year of high school. I think about all the firsts you have missed in the last 5 years; your first big Homecoming dance, your first kiss, your first time driving a car, and maybe your first job. I imagine you would be deciding your next step as you get ready to enter “adulthood”- what college should I attend ? What career do I want? Where will life take me?
But you never got to ask those questions or experience those firsts, your life was cut too short on that sunny crisp fall day 5 years ago in October. And that’s when you came into my life and became a part of me...I will never forget that day. At just 12 years old you breathed your last breath and then through a miracle you breathed life back into my failing tired body. That’s remarkable Joshua, you saved me. Did you ever think in your short 12 years on this earth that you would save others ? What a hero you are!
I will never take your lungs for granted Joshua, I promise you that. It’s really hard sometimes Joshua and some do not understand the magnitude of your gift- the gift of life. But I understand it and as we breathe together I will forever recognize you and your lungs allowing me to take a deep breath, to talk without gasping, and to live without struggling for air.
Your momma and family must be so sad without you but I hope they will find a little peace knowing I’m working really hard to keep us going. I will honor your gift every day, every hour, every minute until we take our last breath together. I will help you experience things that you were unable to do in those 12 short years you were here on earth.
Do you know I have a celebration every year for you? It’s a celebration of life, a time to celebrate our breathing together, and a time to give thanks. But within the celebration of surviving another year, I feel such sadness for you and your family. I know life is precious but still some do not understand that. Life isn’t about rushing around, or worrying about every little detail, or stressing about work and extracurricular activities ——- it’s about being present, appreciating your surroundings, loving one another, and living each day like it’s your last. I get out of bed each day and thank God for what he has done for us and attempt to live life with a purpose- all because of you- a boy I’ve never met, a boy that didn’t get to become a teenager or a man. A boy who didn’t get to experience all of life’s roller coaster ride of triumphs and devastation. A boy whose physical body is gone yet remains in me breathing in and out for me. A boy gone too soon.
Life is so precious Joshua and in an instant it can vanish. I guess that may sound cliche but the reality it’s true and I want people to realize - don’t sweat the small stuff, be grateful, be kind, and BREATHE!
Thank you Joshua. Thank you to your mom, dad, and family that want nothing more to hug you, talk to you, and be with you again. Let’s keep doing life together, breathing in and out, in and out, in and out, in and out........................................................................................................................................
💚💚💚💚💚💚💚💚💚💚💚💚💚💚💚💚💚💚💚💚💚💚💚💚💚💚💚💚💚💚💚
My life with B.O. :Bronchiolitis Obliterans not body odor :)
Autoimmune Bronchiolitis Obliterans, Lung Transplant journey,Joyce Jensen
Thursday, October 10, 2019
Monday, October 10, 2016
2 years
Wow!! It's been 2 years since my transplant! And it's been a bit over 6 months since my last blog; that wasn't deliberate but my first year update blog took a lot out of me. I still can't go back to that blog post-- it's too hard to relive. And what I'm about to discuss is also intensely personal and difficult to put out there.
When a transplant patient makes it to their anniversary date it is a big accomplishment especially for lungs (highest failure rate of any organ). It's natural to think back to the day you received the call, the surgery, and for me all the setbacks I had. I remember the day as if it just happened, even as I'm sitting here in Madison awaiting to go to my appointments the weather is exactly the same as it was 2 years ago. Eerily the same... the sun is shining, the air is crisp yet warm, a slight breeze. Isn't it amazing how some things trigger our memory? Last year the weather was also exactly the same, I know the Mighty One continues to watch over me and perhaps the weather is a way to remind me He is always present through the good and bad. Perhaps it also is a sign from my guardian angel who happened to lose his life on this day to save mine.
My guardian angel is a 12 year old boy whose parents graciously allowed him to live in others. And I am one of those blessed others. I never expected to hear from my donors family, it's just not something that happens in most cases. The videos I share on my page or what TV shows is not the norm. I received my letter on my 1 year lungaversary and when I saw a picture of my guardian angel and learned he was only 12, I was stunned. When I was on the list awaiting my call I prayed for healthy lungs, a child's lungs were never in my thought process. I knew it happened but never thought that it would happen with me.
My guardian angel is named Josh and his father was gracious enough to send me a letter about Josh and who Josh was a person. Josh was an active 12 year old boy who was a Boy Scout, loved to be outdoors, was inventive, and loved his dogs. (Josh had a dog named Snoopy and so do we)
I've been asked if some of my habits have changed since transplant (there has been research regarding recipients taking on new mannerisms/liking new foods that prior to transplant they didn't, and developing new talents from donated organs due to unique cells/DNA that come with transplanted organs). As a recipient you are not told anything about your donor-- and believe me I tried to question/break all the transplant team down. However I knew that my donor was male; I don't know how I just did. I've also noticed after transplant I like cheese much more, I'm the weirdo that would peel cheese off of pizza and now I don't. I'm not inventive like Josh however I was a Girl Scout.
As I awoke this morning I thought of Josh and his family and how they gave the ultimate gift of life. Today has a different meaning for them; hug your children a little tighter, be a bit kinder to one another, and live life for there are no guarantees in this roller coaster of life.
RIP Josh -my guardian angel; I will make you proud.
LIVE LIFE LOVE LIFE GIVE LIFE
When a transplant patient makes it to their anniversary date it is a big accomplishment especially for lungs (highest failure rate of any organ). It's natural to think back to the day you received the call, the surgery, and for me all the setbacks I had. I remember the day as if it just happened, even as I'm sitting here in Madison awaiting to go to my appointments the weather is exactly the same as it was 2 years ago. Eerily the same... the sun is shining, the air is crisp yet warm, a slight breeze. Isn't it amazing how some things trigger our memory? Last year the weather was also exactly the same, I know the Mighty One continues to watch over me and perhaps the weather is a way to remind me He is always present through the good and bad. Perhaps it also is a sign from my guardian angel who happened to lose his life on this day to save mine.
My guardian angel is a 12 year old boy whose parents graciously allowed him to live in others. And I am one of those blessed others. I never expected to hear from my donors family, it's just not something that happens in most cases. The videos I share on my page or what TV shows is not the norm. I received my letter on my 1 year lungaversary and when I saw a picture of my guardian angel and learned he was only 12, I was stunned. When I was on the list awaiting my call I prayed for healthy lungs, a child's lungs were never in my thought process. I knew it happened but never thought that it would happen with me.
My guardian angel is named Josh and his father was gracious enough to send me a letter about Josh and who Josh was a person. Josh was an active 12 year old boy who was a Boy Scout, loved to be outdoors, was inventive, and loved his dogs. (Josh had a dog named Snoopy and so do we)
I've been asked if some of my habits have changed since transplant (there has been research regarding recipients taking on new mannerisms/liking new foods that prior to transplant they didn't, and developing new talents from donated organs due to unique cells/DNA that come with transplanted organs). As a recipient you are not told anything about your donor-- and believe me I tried to question/break all the transplant team down. However I knew that my donor was male; I don't know how I just did. I've also noticed after transplant I like cheese much more, I'm the weirdo that would peel cheese off of pizza and now I don't. I'm not inventive like Josh however I was a Girl Scout.
As I awoke this morning I thought of Josh and his family and how they gave the ultimate gift of life. Today has a different meaning for them; hug your children a little tighter, be a bit kinder to one another, and live life for there are no guarantees in this roller coaster of life.
RIP Josh -my guardian angel; I will make you proud.
LIVE LIFE LOVE LIFE GIVE LIFE
Thursday, March 10, 2016
Expiration Date...
Expiration date, everything has one--milk, cereal, eggs, make-up, and human life. The big difference is there is no date stamped on my forehead however I know its sooner than most. At different times during my journey this weighs on me heavily. And for some reason its been weighing on me again lately.
Maybe its because I have a child who is growing daily and I think of his future-graduation day, wedding day, grandkids and the stark reality is that I will probably not see that.
Maybe its because the majority of the patients I see are over 60 and many are well into their 80s and 90s--doing well and enjoying life. And I think what a privilege it is to grow old.
Or maybe its because I have daily reminders in the handful of meds I take throughout the day.
You see I've said this before, life is short. Life is shorter for me. I still encounter people who don't understand transplant life with lungs. Many think everything is cured. This transplant is not a cure, it bought me some time. These transplanted lungs will fail. It is true that I don't know when but I do know they will.
The statistics have not changed, at 5yrs it is still only 50% survival rate. I believe the longest survivor in the world is 20yrs out, but there are not many that make it there. Its overwhelming to think about.
I am well aware that no one knows when they will die but the hard fact is that most of you will live well into your 70s, 80s, and even 90s-you Dutchies :) . I don't have that.
Most of you will celebrate your golden years with your spouse and enjoy retirement. I don't have that.
Most of you don't think about death. I don't have that.
No, I don't have a crystal ball, I just have the scary statistics that have been laid out before me. Sure I will attempt to prove them wrong, but a fact is a fact.
I haven't stopped fighting, its a daily battle but this is my reality.
I will continue the journey whether its for 1 more year or 10 more years. I have a family to be around for and I have a 12year old boy and his family to honor who gave me the gift of life.
LIFE--------make the most of it, don't take it for granted, and give of yourself.
Live Life, Love Life, Give Life
Maybe its because I have a child who is growing daily and I think of his future-graduation day, wedding day, grandkids and the stark reality is that I will probably not see that.
Maybe its because the majority of the patients I see are over 60 and many are well into their 80s and 90s--doing well and enjoying life. And I think what a privilege it is to grow old.
Or maybe its because I have daily reminders in the handful of meds I take throughout the day.
You see I've said this before, life is short. Life is shorter for me. I still encounter people who don't understand transplant life with lungs. Many think everything is cured. This transplant is not a cure, it bought me some time. These transplanted lungs will fail. It is true that I don't know when but I do know they will.
The statistics have not changed, at 5yrs it is still only 50% survival rate. I believe the longest survivor in the world is 20yrs out, but there are not many that make it there. Its overwhelming to think about.
I am well aware that no one knows when they will die but the hard fact is that most of you will live well into your 70s, 80s, and even 90s-you Dutchies :) . I don't have that.
Most of you will celebrate your golden years with your spouse and enjoy retirement. I don't have that.
Most of you don't think about death. I don't have that.
No, I don't have a crystal ball, I just have the scary statistics that have been laid out before me. Sure I will attempt to prove them wrong, but a fact is a fact.
I haven't stopped fighting, its a daily battle but this is my reality.
I will continue the journey whether its for 1 more year or 10 more years. I have a family to be around for and I have a 12year old boy and his family to honor who gave me the gift of life.
LIFE--------make the most of it, don't take it for granted, and give of yourself.
Live Life, Love Life, Give Life
Tuesday, October 20, 2015
I made it a year!! Lets look back...
I celebrated my 1yr lungaversary 10-10-15!!!! Wowee!! (Imagine me doing cartwheels)
When the weather starts to change in September, memories start creeping back as well. And many of those memories from my early transplant days are not easy to go back to. I think that's why its taking me a bit to start to write this, I've had time but just couldn't do it. I'm having trouble even as I'm typing now. This is hard, this is very hard.
The first 6mos after my double lung transplant were not smooth, they did not go as everyone expected, and because of this I do believe I have some post traumatic stress from those months.
I'm going to go back month by month and try and write a synopsis of the last year--anyone that was a part of this feel free to leave comments about what you remember.
I will be posting very personal pics that are not easy to share and to be honest I have trouble looking at them still.
Ok, here goes...(GULP!) Warning: It will be long.
October 10, 2014-a Friday
We just moved into our current house 3wks ago--things are a mess, boxes are everywhere, and tons of errands to run related to moving/changing address, etc. I met Greg at the secretary of states office on his lunch hour and we were in line forever to change our address on our drivers license. We were walking out after ~1hr wait, it was about 1145 am. It was bright, it was sunny, and pretty warm for October. My phone rang, I looked down and saw the 608 area code (Madison, WI), I wasn't expecting a call from my coordinator but knew I had to answer. I don't even remember the persons name but they asked for Joyce Jensen -- I said that's me--she said something about "We have lungs and the surgeon has determined you are the best match." I said something along the lines--'Are you sure he means ME??!?! They are a match for ME????" She said-'Yes, do you accept these lungs?" My mind is racing, I'm flagging Greg over as he's about to get in his car. I reply, "Yes, I accept" She then tells me something about getting there in a certain time, Can I do that? My mind is going crazy-I tell her I have to call my pilot. I call Randy-he answers right away, asks if I've called Herb (the other pilot), I'm like No-I'm still in shock and he was the first person I called. Randy says he will call Herb. I'm quickly calling other people, Greg is calling other people, Randy calls back -Herb is all set and they both are heading to the airport. Everyone is answering the phone just like they are suppose to. This is literally happening all in a matter of MINUTES!! I call Wisc back-I tell them my transportation is all set. I am jumping in my car--I haven't eaten lunch-Wisc has told me I can't eat. I'm really not hungry-I'm just rushing to get home, still making phone calls, still feeling like I'm on speed.
I get home, I'm thinking I have to shower and shave my legs--who knows when I'll get to do that again! (Little did I know it would be MONTHS before I showered again unencumbered) My phone is blowing up with texts, I cant stop and read them-we have to get to the airport! I think about Eric-he gets out of school at 3:30--we won't be able to say good-bye. That was difficult and it still saddens me as I'm typing this because it would be many weeks until I saw him again.
I can't find my transplant binder I'm suppose to bring with me, we have a suitcase already packed and ready. Where is this damn binder?? I give up my search and get to the car. We make it to the Riverview Airport a bit over a hour from when we get the call. Randy and Herb are there and ready. Mehgan and Scott are there (Mehgan was flying over with us, however she was not as ready as our trusty pilots to fly those bright blue October skies). You see, both of us had discussed our fear of getting into this tiny plane and flying over the huge Lake Michigan--you can imagine where one's thoughts go.
I'm not sure why Greg is so confident with the thumbs up sign, Im of course doing something silly, and you can see Mehgan's look of fear. See we were very cozy inside this plane, and I remember it being very loud inside as well. We arrived safely-the weather was perfect and it was ~1hr 15min ride (Thank you Randy and Herb--they are very capable with tons of experience) and we hurried out of the plane and into our waiting cab. The cabbie rushed us to the hospital--I really don't remember much of the cab ride. We went to admissions-everything was ready and we were there for a matter of minutes and the admissions lady escorted us to the floor.
I remember the charge nurse Alice greeting us with a big hello and a personal escort to my room. I liked Alice immediately and she helped calm my insides with her warmth-I found out later during a different admission that Alice and I were kindred spirits when we sang together loudly in my room and the neighboring patient complained. The nerve we said!
Wisconsin is 1 hour behind Michigan in time and it was about 3pm there. There were so many people in and out-I couldn't keep track. I was asking EVERYONE about my donor--how old were they, where were they from, was it male or female? I couldn't get any info, some may not want to know but I wanted to know something about these lungs that were about to become part of me. Finally, one of the cardiothoracic fellows came in and told me they were coming from central Wisconsin and surgery would be around 8pm. Believe me, I tried to get info!
Throughout all this, I had to take a Betadine shower from head to toe, give a trillon vials of blood, and do an enema. (Sorry you had to help with that Mehgan!)
At about 8pm they wheeled me down to the OR-the first thing I saw was a bunch of people lining the hallway in scrubs. Wow-things just got very real-these were people all involved in my surgery. I also go to meet my Friday night date--my cardiothoracic surgeon Dr Maloney. I had met the other surgeon during my eval, Dr Maloney was smaller than I expected for a surgeon about to cut me in half. I asked him if he had eaten and had caffeine-I didn't want him passing out before our big 8hr date! I was in this holding area for what seemed like 5-10min then said good-bye to Mehgan and Greg and was off to OR.
I told everyone along the way that I was a difficult intubation because of my fused cervical vertebrae (which means very little to no hyperflexion of my neck) and that I take A LOT of medicine to knock me out. During other procedures, I've been called a baby hippo because of the amount of sedative it takes to knock me out. I'm not sure why--I've never been on chronic pain meds before...part of the complicated puzzle that I am I guess.
The next 24-48hrs are much of a blur for me. This is where having people comment would be great. The surgery went well I'm told, it lasted about 8hrs or so and I believe I was out of the OR at 4am Saturday. The transplant team likes to extubate (remove breathing tube) in the first 24hrs (less risk of infection) but they kept my in because I was such a difficult intubation and to be safe they kept my tube in until Sun evening. I would awaken at times while being on the ventilator and was VERY hard. I heard stuff like, ' her pressure is low, she needs more blood.' I barely remember family and friends coming in.
At some point I was less sedated and remember communicating by writing out words on people's palms. This didn't work out that great. At this time they also lowered some of the vent settings and I was breathing more on my own but after awhile I told the respiratory therapist it was too hard so they set the ventilator back to do all my breathing for me. Personally, being awake and aware of a tube down my throat was the worse experience for me. I HATED every moment. I guess they couldn't sedate me more because my blood pressure was too low. I know this is one of the memories that it is very difficult to dwell on and causes me anxiety. I never want to be on a ventilator again.
Not a pretty sight...(Intubated)
There are lines and tubes everywhere. I had 4 chest tubes, multiple IV lines including one in my neck, and a catheter.
The team wants you up and walking as soon as possible. I remember them saying I had to sit in a chair for 3hrs and I thought they were nuts--it was exhausting. On one of my walks, my transplant doc (Dr Cornwell) came by to say hi. I said it feels like I've been hit by a bus and he gently nodded and said thats what many of our patients say. I don't remember hearing this before transplant.
Soon after extubation.
My first walk
On Tuesday I was sitting up, trying to get the many pills that were now going to be my norm. I wasn't feeling very confident in my swallowing after my prolonged intubation (vocal cords were swollen) and was taking it slow. I swallowed one larger pill that I wasn't feeling too good about and lo and behold that bugger got stuck and I was choking. My sister in law screamed my name, I was desperately trying to swallow--praying and finally it went down. The nurse came and took away the pills and ordered a swallow study. I of course failed and a feeding tube was my next torture session.
During this stay in the hospital, I remember lack of sleep, the start of diarrhea (from some of the immunosuppressants and my tube feeding), and blurred/decreased vision and other visual disturbances from the massive dose of steroids I was receiving. I would be looking at the wallpaper and the flowers would be spinning or the design of someone's pants would be moving--all common with high dose steroids.
I also remember coughing with a bit of wheeze--the docs were concerned about the right lower lobe. Dr Maloney said it looked 'heavy', I asked if from trauma and he replied no. So it must have come with questionable infection. I've been asked-why did they transplant it then? All I can say, I'm not the expert, they know what they are doing and I knew God was in control of all this. Everything happens for a reason and sometimes we never know that reason.
I was getting a lot of bronchs, they went in and cleaned out as many secretions as they could. I tried to cough them up but I was so weak-I remember one pulmonologist telling me that I wouldn't have been able to cough them up because they were too deep.
I was trying to do everything they wanted, it was such an effort. The respiratory therapist would make his rounds and make me do my breathing exercises--ugh it was so hard! That 10min felt like forever-and again I was so sleep deprived that my body was exhausted! I rarely slept for more than 1hr at a time--the steroids along with the constant interruptions --the chest xray people came at 4am everyday! The residents and interns make their rounds before the attending--so many were there at 6am. And those rooms don't get dark enough--theres always light shining in somewhere.
There was one night that I got up to hurry to the bathroom (diarrhea), I had still so many tubes (down to 3chest tubes) and I didn't make it in time. How embarrassing! Plus I was a bit delusional and making up weird stories--just ask Greg. Sleep deprivation and high dose steroids with at least a dozen other meds= bad news bears. There is something called sleep psychosis and I was in that territory.
But, I was getting a bit stronger everyday. I begged daily to have the chest tubes removed--most of the time they are all gone in 4-5days. But I still had too much drainage or a lung wasn't fully inflated.
The feeding tube was driving me nuts, I couldn't wait for my repeat swallow study. I was doing my swallowing exercises and was determined to pass that thing. I think I had that tube in for about a week. By this time, I was getting restless from being in the hospital, I wanted to get out of there. Some nice nurse asked me if I would like my hair washed after about a week and I was so excited. I think I wrote about her in a previous blog.
Yea for clean hair!
Oct 22--Eric had a few days off from school so my mom brought him over to Wisconsin.
On Oct 23, I finally got to be discharged to a local hotel, I had to go with 2 chest tubes but I got to leave the hospital! I was beyond excited. Those hospital beds are anything but comfortable and no hospital food--wahoo! I can't say I was very hungry but anything but hospital food is good news. To be fair, UW did have a pretty good selection of food.
Discharge Day!!!!
I didn't get to leave the hospital until after dinner, I had to wait forever for pharmacy to get my meds ready-but I was leaving and thats all that mattered.
We stayed at a nice Marriott Extended Stay--the bed was heaven! The staff were so nice. My exercise would be walking around the 2nd floor. I would go for ~ 6minutes but felt like forever. I was also going to pulmonary rehab 3x/week at the hospital and my transplant coordinator would come see me then as well. The drive from the hotel to the hospital was about 20min but I was still a bit nauseous with car movement and would have to semi-lie while riding. During one of my pulm rehab sessions, she checked my blood pressure and it was 80/40--I got to get rid of my water pill and lower one of the others. My heart rate stayed high after transplant and they put me on a med to lower that but can also lower the BP.
While back at my extended stay, one of the receptionists asked about my chest tubes. I told her I had a lung transplant 2wks prior and she said-"Oh my! Shouldn't you be in bed?" I thought that was funny, I guess seeing someone who just had a lung transplant isn't a common occurrence.
While Eric was in town, we went to Target to get his costume. The transplant team encouraged outings. I didn't want to go--I had 2 chest tubes that I was lugging around but I went. I didn't want to be dropped off at the door, it was busy so I walked in from the faraway parking space. I was self conscious from wearing a mask and carrying these nasty containers around. Boy-did I get stares! I wasn't feeling the greatest -was feeling a bit lightheaded and definitely awkward. I couldn't take the stares anymore and my mom and I left while Greg and Eric picked out the costume. I was determined not to pass out-I made it back to the car, laid all the way back in the seat, and focused on my breathing. I wasn't going to do that again anytime soon!
I continued with my pulm rehab and follow up appts, asking when I could go home. Not yet, not yet was what I kept hearing. Greg had been with me daily at this point, I encouraged him to go home for the weekend for Halloween. Eric would be excited and he had some stuff he needed to do renovation wise before I came home (remember we just moved in). He reluctantly went after much reassurance from myself and Mehgan. I knew he needed to get away. This wasn't easy for anyone involved, he had been sleeping on a cot for 2wks then by my side at the hotel. Thankfully, his work was being supportive.
November
I don't know the date, but sometime in November I had a follow up with Dr Maloney. They decided they were going to try and pull one of the two chest tubes. They asked me to come back later that day for a follow up chest xray. I had my CXR and got a call a few hours later from one of the residents--your lung is collapsed-we need to put the chest tube back in. I didn't feel more short of breath, hmmmm, ok. I went back into the hospital that day, had the chest tube placed early evening and had to stay overnight. ERGH! At this same time, they decided to bronch me again in the AM and after I could go back to the hotel.
A few days later, on a Saturday, I got a call from one of the on call pulmonologists. My culture from the bronch grew out pseudomonas--this is a very nasty bacteria. He needed me to start on oral antibiotics ASAP. The following Monday, I had a follow up in the transplant clinic--my CXR was looking weird in the right lower lobe so they decided to get a CT scan. I told my transplant doc I had been feeling good and really needed to get home, it had been a month and I was desperately homesick. First we had to do the CT--I got the scan done around 4pm and got a call from Dr Cornwell himself about a hour later (never a good sign). He told me the CT scan didn't look good-the right lower lobe was necrotic (starting to die) and full of infection. I needed to be admitted the next day to start on IV antibiotics and I needed to go back into surgery to have that lobe removed. I was crushed! I was just starting to feel better, get stronger, and had to take huge steps backwards. I WANTED TO GO HOME!!! We were thinking we would be leaving Madison in a day or two instead we had to go back into the hospital--it was a definite blow.
We woke up the next AM, stuff all packed up to check out of our home away from home, we were waiting for Wisc to call with further instructions. I knew they would be calling first thing--I looked at my phone and it was dead. Couldn't turn it on, blank screen--DEAD! Come on! What else! Greg called the transplant team to let them know to call his phone and they said they had already called me and left a message. Thankfully there was a Verizon store close to the hotel and we stopped there on the way to the hospital--it needed a hard reboot-something weird that Iphones do ocassionally.
We went back into the hospital on 11-10, I was still feeling kinda low. I had worked so hard and now I had to go back to surgery. And this was very serious, I had a serious infection with an immunocomprised (and still sorta in shock) body and a dying lung.
They wanted me on IV antibiotics for a week before they took me to surgery--needed to kill some of the infection. I got a PICC line for the antibiotics. Dr Maloney consulted a plastic surgeon as well for the upcoming surgery--the plan was to make an incision down the side of my chest to remove the lung, they then wanted to put a muscle flap in that area to fill it in. This is where plastics came in-they would remove some of my ribs and bring some muscles from behind my shoulder blade down into that space. Why do they have to remove the ribs to do this? Because if the muscle is placed between the ribs it could get pinched and cut off its blood supply and subsequently die. Someone from anesthesia came and talked to me about an epidural--I was all about it if I didn't have to feel the post-op pain.
Nov 17: Surgery day -Right lower lobectomy with muscle flap
I was not looking forward to being intubated again, it terrified me out of everything. I only remember being in the OR holding room and talking with anesthesia and making sure they know I was a difficult intubation. The next thing I know is that I was back in the ICU on a vent. I was up all night looking at the light completely aware of that horrible tube down my throat. Sure I was in and out, but I can distinctly remember biting on that tube, hands tied down, the nurse telling me not to bite on the tube, my lips were so dry, watching the clock and praying for the morning to hurry up and get here. It was horrible-thats the only adjective that clearly describes my feelings.
Around 6am the next day, the said they were going to take the tube out. Was I ready? A resounding YES! They said when they pulled it out to make sure to cough and not swallow any secretions as they could go in my lungs. Man I was scared of doing something wrong. I don't remember being this awake when I was extubated after the transplant. Please Lord help me! I did it and thankfully all went ok. They gave me my incentive spirometer to work my lungs and I did that guy faithfully--I didn't want to see another intubation tube for the rest of my life!
The epidural wasn't working and I remember the pain being pretty difficult. Since the epidural wasn't working I just had them pull it the next day.
The first time I looked in the mirror and saw where my ribs were removed, I cried. I was shocked, this huge crater in the side of my chest was not what I was expecting. I don't know what I was expecting but this wasn't it. I felt deformed. I still have trouble looking at it. So the pics below take some courage to post because they are not pretty but they are me. I post because I want you to see what I've survived.
The main scar from the transplant surgery--armpit to armpit-the scars in front lower right are from chest tubes
The right side where ribs are removed, also can see where chest tubes were
right side-additional view-that incision goes up and down starting right under my armpit
When the weather starts to change in September, memories start creeping back as well. And many of those memories from my early transplant days are not easy to go back to. I think that's why its taking me a bit to start to write this, I've had time but just couldn't do it. I'm having trouble even as I'm typing now. This is hard, this is very hard.
The first 6mos after my double lung transplant were not smooth, they did not go as everyone expected, and because of this I do believe I have some post traumatic stress from those months.
I'm going to go back month by month and try and write a synopsis of the last year--anyone that was a part of this feel free to leave comments about what you remember.
I will be posting very personal pics that are not easy to share and to be honest I have trouble looking at them still.
Ok, here goes...(GULP!) Warning: It will be long.
October 10, 2014-a Friday
We just moved into our current house 3wks ago--things are a mess, boxes are everywhere, and tons of errands to run related to moving/changing address, etc. I met Greg at the secretary of states office on his lunch hour and we were in line forever to change our address on our drivers license. We were walking out after ~1hr wait, it was about 1145 am. It was bright, it was sunny, and pretty warm for October. My phone rang, I looked down and saw the 608 area code (Madison, WI), I wasn't expecting a call from my coordinator but knew I had to answer. I don't even remember the persons name but they asked for Joyce Jensen -- I said that's me--she said something about "We have lungs and the surgeon has determined you are the best match." I said something along the lines--'Are you sure he means ME??!?! They are a match for ME????" She said-'Yes, do you accept these lungs?" My mind is racing, I'm flagging Greg over as he's about to get in his car. I reply, "Yes, I accept" She then tells me something about getting there in a certain time, Can I do that? My mind is going crazy-I tell her I have to call my pilot. I call Randy-he answers right away, asks if I've called Herb (the other pilot), I'm like No-I'm still in shock and he was the first person I called. Randy says he will call Herb. I'm quickly calling other people, Greg is calling other people, Randy calls back -Herb is all set and they both are heading to the airport. Everyone is answering the phone just like they are suppose to. This is literally happening all in a matter of MINUTES!! I call Wisc back-I tell them my transportation is all set. I am jumping in my car--I haven't eaten lunch-Wisc has told me I can't eat. I'm really not hungry-I'm just rushing to get home, still making phone calls, still feeling like I'm on speed.
I get home, I'm thinking I have to shower and shave my legs--who knows when I'll get to do that again! (Little did I know it would be MONTHS before I showered again unencumbered) My phone is blowing up with texts, I cant stop and read them-we have to get to the airport! I think about Eric-he gets out of school at 3:30--we won't be able to say good-bye. That was difficult and it still saddens me as I'm typing this because it would be many weeks until I saw him again.
I can't find my transplant binder I'm suppose to bring with me, we have a suitcase already packed and ready. Where is this damn binder?? I give up my search and get to the car. We make it to the Riverview Airport a bit over a hour from when we get the call. Randy and Herb are there and ready. Mehgan and Scott are there (Mehgan was flying over with us, however she was not as ready as our trusty pilots to fly those bright blue October skies). You see, both of us had discussed our fear of getting into this tiny plane and flying over the huge Lake Michigan--you can imagine where one's thoughts go.
I'm not sure why Greg is so confident with the thumbs up sign, Im of course doing something silly, and you can see Mehgan's look of fear. See we were very cozy inside this plane, and I remember it being very loud inside as well. We arrived safely-the weather was perfect and it was ~1hr 15min ride (Thank you Randy and Herb--they are very capable with tons of experience) and we hurried out of the plane and into our waiting cab. The cabbie rushed us to the hospital--I really don't remember much of the cab ride. We went to admissions-everything was ready and we were there for a matter of minutes and the admissions lady escorted us to the floor.
I remember the charge nurse Alice greeting us with a big hello and a personal escort to my room. I liked Alice immediately and she helped calm my insides with her warmth-I found out later during a different admission that Alice and I were kindred spirits when we sang together loudly in my room and the neighboring patient complained. The nerve we said!
Wisconsin is 1 hour behind Michigan in time and it was about 3pm there. There were so many people in and out-I couldn't keep track. I was asking EVERYONE about my donor--how old were they, where were they from, was it male or female? I couldn't get any info, some may not want to know but I wanted to know something about these lungs that were about to become part of me. Finally, one of the cardiothoracic fellows came in and told me they were coming from central Wisconsin and surgery would be around 8pm. Believe me, I tried to get info!
Throughout all this, I had to take a Betadine shower from head to toe, give a trillon vials of blood, and do an enema. (Sorry you had to help with that Mehgan!)
At about 8pm they wheeled me down to the OR-the first thing I saw was a bunch of people lining the hallway in scrubs. Wow-things just got very real-these were people all involved in my surgery. I also go to meet my Friday night date--my cardiothoracic surgeon Dr Maloney. I had met the other surgeon during my eval, Dr Maloney was smaller than I expected for a surgeon about to cut me in half. I asked him if he had eaten and had caffeine-I didn't want him passing out before our big 8hr date! I was in this holding area for what seemed like 5-10min then said good-bye to Mehgan and Greg and was off to OR.
I told everyone along the way that I was a difficult intubation because of my fused cervical vertebrae (which means very little to no hyperflexion of my neck) and that I take A LOT of medicine to knock me out. During other procedures, I've been called a baby hippo because of the amount of sedative it takes to knock me out. I'm not sure why--I've never been on chronic pain meds before...part of the complicated puzzle that I am I guess.
The next 24-48hrs are much of a blur for me. This is where having people comment would be great. The surgery went well I'm told, it lasted about 8hrs or so and I believe I was out of the OR at 4am Saturday. The transplant team likes to extubate (remove breathing tube) in the first 24hrs (less risk of infection) but they kept my in because I was such a difficult intubation and to be safe they kept my tube in until Sun evening. I would awaken at times while being on the ventilator and was VERY hard. I heard stuff like, ' her pressure is low, she needs more blood.' I barely remember family and friends coming in.
At some point I was less sedated and remember communicating by writing out words on people's palms. This didn't work out that great. At this time they also lowered some of the vent settings and I was breathing more on my own but after awhile I told the respiratory therapist it was too hard so they set the ventilator back to do all my breathing for me. Personally, being awake and aware of a tube down my throat was the worse experience for me. I HATED every moment. I guess they couldn't sedate me more because my blood pressure was too low. I know this is one of the memories that it is very difficult to dwell on and causes me anxiety. I never want to be on a ventilator again.
Not a pretty sight...(Intubated)
There are lines and tubes everywhere. I had 4 chest tubes, multiple IV lines including one in my neck, and a catheter.
The team wants you up and walking as soon as possible. I remember them saying I had to sit in a chair for 3hrs and I thought they were nuts--it was exhausting. On one of my walks, my transplant doc (Dr Cornwell) came by to say hi. I said it feels like I've been hit by a bus and he gently nodded and said thats what many of our patients say. I don't remember hearing this before transplant.
Soon after extubation.
My first walk
On Tuesday I was sitting up, trying to get the many pills that were now going to be my norm. I wasn't feeling very confident in my swallowing after my prolonged intubation (vocal cords were swollen) and was taking it slow. I swallowed one larger pill that I wasn't feeling too good about and lo and behold that bugger got stuck and I was choking. My sister in law screamed my name, I was desperately trying to swallow--praying and finally it went down. The nurse came and took away the pills and ordered a swallow study. I of course failed and a feeding tube was my next torture session.
Check out that neck-I was relieved to get that line out
I also remember coughing with a bit of wheeze--the docs were concerned about the right lower lobe. Dr Maloney said it looked 'heavy', I asked if from trauma and he replied no. So it must have come with questionable infection. I've been asked-why did they transplant it then? All I can say, I'm not the expert, they know what they are doing and I knew God was in control of all this. Everything happens for a reason and sometimes we never know that reason.
I was getting a lot of bronchs, they went in and cleaned out as many secretions as they could. I tried to cough them up but I was so weak-I remember one pulmonologist telling me that I wouldn't have been able to cough them up because they were too deep.
I was trying to do everything they wanted, it was such an effort. The respiratory therapist would make his rounds and make me do my breathing exercises--ugh it was so hard! That 10min felt like forever-and again I was so sleep deprived that my body was exhausted! I rarely slept for more than 1hr at a time--the steroids along with the constant interruptions --the chest xray people came at 4am everyday! The residents and interns make their rounds before the attending--so many were there at 6am. And those rooms don't get dark enough--theres always light shining in somewhere.
There was one night that I got up to hurry to the bathroom (diarrhea), I had still so many tubes (down to 3chest tubes) and I didn't make it in time. How embarrassing! Plus I was a bit delusional and making up weird stories--just ask Greg. Sleep deprivation and high dose steroids with at least a dozen other meds= bad news bears. There is something called sleep psychosis and I was in that territory.
But, I was getting a bit stronger everyday. I begged daily to have the chest tubes removed--most of the time they are all gone in 4-5days. But I still had too much drainage or a lung wasn't fully inflated.
The feeding tube was driving me nuts, I couldn't wait for my repeat swallow study. I was doing my swallowing exercises and was determined to pass that thing. I think I had that tube in for about a week. By this time, I was getting restless from being in the hospital, I wanted to get out of there. Some nice nurse asked me if I would like my hair washed after about a week and I was so excited. I think I wrote about her in a previous blog.
Yea for clean hair!
Oct 22--Eric had a few days off from school so my mom brought him over to Wisconsin.
On Oct 23, I finally got to be discharged to a local hotel, I had to go with 2 chest tubes but I got to leave the hospital! I was beyond excited. Those hospital beds are anything but comfortable and no hospital food--wahoo! I can't say I was very hungry but anything but hospital food is good news. To be fair, UW did have a pretty good selection of food.
Discharge Day!!!!
I didn't get to leave the hospital until after dinner, I had to wait forever for pharmacy to get my meds ready-but I was leaving and thats all that mattered.
We stayed at a nice Marriott Extended Stay--the bed was heaven! The staff were so nice. My exercise would be walking around the 2nd floor. I would go for ~ 6minutes but felt like forever. I was also going to pulmonary rehab 3x/week at the hospital and my transplant coordinator would come see me then as well. The drive from the hotel to the hospital was about 20min but I was still a bit nauseous with car movement and would have to semi-lie while riding. During one of my pulm rehab sessions, she checked my blood pressure and it was 80/40--I got to get rid of my water pill and lower one of the others. My heart rate stayed high after transplant and they put me on a med to lower that but can also lower the BP.
While back at my extended stay, one of the receptionists asked about my chest tubes. I told her I had a lung transplant 2wks prior and she said-"Oh my! Shouldn't you be in bed?" I thought that was funny, I guess seeing someone who just had a lung transplant isn't a common occurrence.
While Eric was in town, we went to Target to get his costume. The transplant team encouraged outings. I didn't want to go--I had 2 chest tubes that I was lugging around but I went. I didn't want to be dropped off at the door, it was busy so I walked in from the faraway parking space. I was self conscious from wearing a mask and carrying these nasty containers around. Boy-did I get stares! I wasn't feeling the greatest -was feeling a bit lightheaded and definitely awkward. I couldn't take the stares anymore and my mom and I left while Greg and Eric picked out the costume. I was determined not to pass out-I made it back to the car, laid all the way back in the seat, and focused on my breathing. I wasn't going to do that again anytime soon!
I continued with my pulm rehab and follow up appts, asking when I could go home. Not yet, not yet was what I kept hearing. Greg had been with me daily at this point, I encouraged him to go home for the weekend for Halloween. Eric would be excited and he had some stuff he needed to do renovation wise before I came home (remember we just moved in). He reluctantly went after much reassurance from myself and Mehgan. I knew he needed to get away. This wasn't easy for anyone involved, he had been sleeping on a cot for 2wks then by my side at the hotel. Thankfully, his work was being supportive.
November
I don't know the date, but sometime in November I had a follow up with Dr Maloney. They decided they were going to try and pull one of the two chest tubes. They asked me to come back later that day for a follow up chest xray. I had my CXR and got a call a few hours later from one of the residents--your lung is collapsed-we need to put the chest tube back in. I didn't feel more short of breath, hmmmm, ok. I went back into the hospital that day, had the chest tube placed early evening and had to stay overnight. ERGH! At this same time, they decided to bronch me again in the AM and after I could go back to the hotel.
A few days later, on a Saturday, I got a call from one of the on call pulmonologists. My culture from the bronch grew out pseudomonas--this is a very nasty bacteria. He needed me to start on oral antibiotics ASAP. The following Monday, I had a follow up in the transplant clinic--my CXR was looking weird in the right lower lobe so they decided to get a CT scan. I told my transplant doc I had been feeling good and really needed to get home, it had been a month and I was desperately homesick. First we had to do the CT--I got the scan done around 4pm and got a call from Dr Cornwell himself about a hour later (never a good sign). He told me the CT scan didn't look good-the right lower lobe was necrotic (starting to die) and full of infection. I needed to be admitted the next day to start on IV antibiotics and I needed to go back into surgery to have that lobe removed. I was crushed! I was just starting to feel better, get stronger, and had to take huge steps backwards. I WANTED TO GO HOME!!! We were thinking we would be leaving Madison in a day or two instead we had to go back into the hospital--it was a definite blow.
We woke up the next AM, stuff all packed up to check out of our home away from home, we were waiting for Wisc to call with further instructions. I knew they would be calling first thing--I looked at my phone and it was dead. Couldn't turn it on, blank screen--DEAD! Come on! What else! Greg called the transplant team to let them know to call his phone and they said they had already called me and left a message. Thankfully there was a Verizon store close to the hotel and we stopped there on the way to the hospital--it needed a hard reboot-something weird that Iphones do ocassionally.
We went back into the hospital on 11-10, I was still feeling kinda low. I had worked so hard and now I had to go back to surgery. And this was very serious, I had a serious infection with an immunocomprised (and still sorta in shock) body and a dying lung.
They wanted me on IV antibiotics for a week before they took me to surgery--needed to kill some of the infection. I got a PICC line for the antibiotics. Dr Maloney consulted a plastic surgeon as well for the upcoming surgery--the plan was to make an incision down the side of my chest to remove the lung, they then wanted to put a muscle flap in that area to fill it in. This is where plastics came in-they would remove some of my ribs and bring some muscles from behind my shoulder blade down into that space. Why do they have to remove the ribs to do this? Because if the muscle is placed between the ribs it could get pinched and cut off its blood supply and subsequently die. Someone from anesthesia came and talked to me about an epidural--I was all about it if I didn't have to feel the post-op pain.
Nov 17: Surgery day -Right lower lobectomy with muscle flap
I was not looking forward to being intubated again, it terrified me out of everything. I only remember being in the OR holding room and talking with anesthesia and making sure they know I was a difficult intubation. The next thing I know is that I was back in the ICU on a vent. I was up all night looking at the light completely aware of that horrible tube down my throat. Sure I was in and out, but I can distinctly remember biting on that tube, hands tied down, the nurse telling me not to bite on the tube, my lips were so dry, watching the clock and praying for the morning to hurry up and get here. It was horrible-thats the only adjective that clearly describes my feelings.
Around 6am the next day, the said they were going to take the tube out. Was I ready? A resounding YES! They said when they pulled it out to make sure to cough and not swallow any secretions as they could go in my lungs. Man I was scared of doing something wrong. I don't remember being this awake when I was extubated after the transplant. Please Lord help me! I did it and thankfully all went ok. They gave me my incentive spirometer to work my lungs and I did that guy faithfully--I didn't want to see another intubation tube for the rest of my life!
The epidural wasn't working and I remember the pain being pretty difficult. Since the epidural wasn't working I just had them pull it the next day.
The first time I looked in the mirror and saw where my ribs were removed, I cried. I was shocked, this huge crater in the side of my chest was not what I was expecting. I don't know what I was expecting but this wasn't it. I felt deformed. I still have trouble looking at it. So the pics below take some courage to post because they are not pretty but they are me. I post because I want you to see what I've survived.
The main scar from the transplant surgery--armpit to armpit-the scars in front lower right are from chest tubes
The right side where ribs are removed, also can see where chest tubes were
right side-additional view-that incision goes up and down starting right under my armpit
left side--chest tube scars, can also see the transplant scar (upper left)
Ok so thats what it looks like today. Last November not so much.
I got out of the hospital Nov 24 with 2 chest tubes (still from lung transplant),a JP drain from my muscle flap site, and a PICC line for IV antibiotics. They were going to reluctantly let me go home to MICHIGAN!!! I was beyond excited. The trip home was long and trying to hide chest tubes in your winter jacket while you used a reststop--lets say interesting. My IV antibiotics were every 6hrs, so at some point I had an antibiotic bag hanging from that handle that is above the door going down the highway. I wonder what people thought if they looked over and saw that.
I also had weekly visiting nurses to draw blood and change my PICC line dressing.
But we made it home 2 days before Thanksgiving and I was grateful for that. I was scheduled to return to Wisc in 3wks.
So I was home finally, tending to daily dressing changes--bathroom sink baths, and still trying to acclimate to these meds. I still didn't feel quite well.
December
It was around Dec 7 or so and I was making dinner. It was annoying with the 2 chest tubes--hanging them on a drawer handle and trying not to trip over the drainage tubes. But I was home!!
As I was flipping the turkey burgers I felt a wetness on the right side of my shirt--what could that be?
I went into the bathroom and the next thing I saw was one of my chest tubes on the floor! Did that just come out of me? Do I shove it back in quickly? Am I going to start feeling short of breath? What do I do with this gaping hole in the side of my chest? These are just a few of my racing thoughts. I called for help and my mom came. We needed to get to the hospital! I called my transplant team and let them know that I was heading to the hospital. An ambulance was coming. While waiting for the ambulance my cardiothoracic surgeon-Dr Maloney called. He asked what happened. I said "Evidently one of your residents doesn't know how to suture in a chest tube" (Residents get the boring jobs at the end of cases including suturing) He wasn't expecting that answer and laughed. I was feeling pretty calm, no breathing trouble-I was good.
He told him to keep him informed, have the ER doc call him, and off I went in an ambulance to Butterworth ER. I was most worried if the lung collapsed and would need the chest tube replaced. If you want speedy service, we all know the ER is not the place. I couldn't believe how long it took to get a CXR done or see a doctor. Evidently a newly transplanted lung patient isn't high priority. Dr Maloney was texting me because he hadn't heard anything. I finally got a CXR-yep lung is collapsed then a CT scan then I was admitted.
Wisc was still worried about the right lower lobe area--the infection was so bad prior to lobectomy that it got into the fluid that surrounds the lung.
I had the chest tube placed late the next day. My own pulmonologist was on call that week and I got to see my first familiar face from my medical team. That was so nice!
I asked daily when I could go home. I was in Butterworth for 3days, I got out on a Friday and had my already scheduled appts for Wisc the following Weds.
We traveled to Wisc and were expecting to travel back home the next day. Packing up all my meds, all the IV stuff, and nebulizer stuff took time. All my meds needed to be taken at very specific times-traveling wasn't very conducive for this.
My first appt was with the infectious disease doc (because of the pseudomonas), my most recent labs showed an elevated white blood cell (WBC) count--this can happen with infection. He didn't seem too concerned because my inflammatory markers were not too high. He wanted me to recheck the CBC later that afternoon. I did that then headed back to the hotel to hook my IV.
I got a call from the transplant team--my WBC were quite elevated, they needed to admit me and work me up for an infection. I had been on IV antibiotics continuously since my November admission/surgery--was there another source of infection?
Devastated wouldn't even describe my feelings at this point. I couldn't go in the hospital again! We packed up all my stuff and headed back to the hospital. I had to submit blood from my PICC line to check for infection as well as a seperate site, a urine sample, and stool samples. My blood cultures were neg, my urine was neg, and my stool was neg for infection. All good news but where was the source of infection? The CT scan of my lungs I had done showed 'pockets' of fluid around the muscle flap site. The next step was to go in under CT scan while the radiologist placed drains into those pockets of fluid. He would obtain fluid samples to send off for testing. This took 2-3hrs.
The testing showed pseudomonas---ugh! Still!!!
I'm not sure how long that hospital stay was. I got to leave but we had return office visits every 2-3wks.
January
I got one of the tubes out-which was triumphant. A few wks later (late Jan) I got the rest of the tubes out and the sutures out from my Nov surgery. WOW! After 3 1/2 months I was finally without drains. The only tube I had left was my PICC line. I could finally shower but would have to wrap the PICC line. But I could shower! I could shower! I could shower! 3 1/2 months of sink sponge baths -finally gone. I could shower! I could shower!
This was a big deal! I could walk without making noise my chest tubes clinking together. I could finally lie on my right side without feeling the prick from my tubes. This was GLORIOUS!
February
I was still struggling with intense diarrhea (7-8x/day) which has been going on for a few mos. It is a known side effect of one of the transplant meds so they lowered the dose. Also being on strong IV antibiotics for so long does not help the gut.
I'm having routine CT scans to watch right lower former lung area -I find out during one of these CTs that the right middle lobe has collapsed ---the infection/trauma overwhelmed this finicky area and he decided to throw in the towel. A bummer indeed--the loss of these 2 lobes will affect my lung function.
On one of my visits back in Wisc the doc tells me we can stop the antibiotics at the end of the week, and get rid of the PICC line.
I will finally be completely drain free!!! Now I can shower without a plastic wrapped right arm (its not the easiest to shampoo with saran wrap from wrist to shoulder). OH GLORIOUS DAY!! WAHHHOOOOOOOO!!!!!!
I'm also working out daily and building up my strength.
March
I return to work for two days a wk-starting at 4hrs each day. I cannot see patients with fever or other respiratory issues. I'm still nervous as it is a doctors office and viruses travel. After the last few mos I'm a bit paranoid and terrified of returning to a hospital.
I wanted my stool checked again for c-diff and I feel something has changed. The testing comes back positive for c-diff. C-diff is a nasty intestinal bacteria, it occurs when all the good bacteria is eaten up and the bad bacteria takes over. I have to start an oral antibiotic x4wks.
I'm getting weekly labs -all is stable. Stable is a word I've come to adore.
April-June
Monthly visits to Wisconsin. I am bronched again in June with another CT. The CT is stable, labs are stable, all is looking good.
Late June-I get a call from Dr Cornwell (remember not a good sign). My fungal culture from my bronch 2wks prior has grown out some weird rare fungus (fusariam) and we need to change my anti-fungal medicine to a stronger one with potentially nasty side effects. (Fungal cultures can take 3-4wks to come back with final results)
Ahhh-just when I thought I was in the clear. I also have to get another CT to look for any fungal growths and get more blood drawn. Sometimes these fungal results can be from a contaminant-clinically I'm well and we have to watch closely.
My CT again looks stable-thank you God!
The transplant team wants me to see Infectious Disease in Wisc.
July
At the end of July I see the Infectious Disease doc, my labs have all been good, my CT did not show any new growths, and I'm feeling fine. All good news. I understand the need to see a patient in person, I just wanna escape ASAP.
The doc decides with above findings that I can stop the newer antifungal and return to the other. She wants another CT in 2mos to eval for any new growths.
August
Working out daily--1hr cardio a day: 12-13 miles on bike 1-2x/wk or treadmill 3.5miles 5-6x/wk
Feeling stronger, working on my paranoia of catching something. I still hear every cough that is in a 5mile radius.
Sept
Repeat CT--stable! I'm so thankful. Labs have been looking good as well.
Every now and then I see others that have had a double lung transplant and their function is 100+% (I know that sounds weird but you can have 110% lung function) or others that have 80, 90% lung function and I will never have that. I went through this massive surgery and won't have what I wanted most--normal lung function. It doesn't seem fair, but I cannot dwell on these thoughts forever. My left lung (I named Charlie) is holding on strong and I will continue to push with my 1 1/3 remaining lungs. I am grateful--I have reached 60% lung function and this is probably the best it will be. I was at 17% at my lowest-I've tripled!! This is huge and so I will focus that.
Oct 2015
I've made it a year!!!!!!!!!!!!!!!!!!!!!!!!!! Its a very big deal. I have my 1yr testing with bronch on 10-12-15 and all looks well. I'm still holding my breath for those fungal cultures but God is in control. Cold/flu/school season are here and I'm admittedly scared.
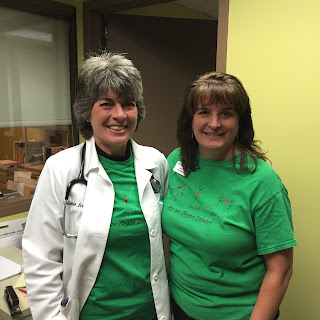
My co-workers surprised me with awesome lungaversary cakes and continue to spread the word about organ donation with T-shirt Tuesday!!
As if I haven't shared enough unflattering pics--sweaty me after treadmill- I will never understand the selfie thing.
I really can't thank everyone enough. This journey has been downright terrifying at times and I couldn't do it without you. I am so grateful for the support and love!
I thank you for the love, the prayers, your time, help around the house, financial support, cards, but most of all for standing by my side.
What have I learned in the past year? My husband is the best-God knew what he was doing when He put Greg in my life. He has stood by me through it all and it isn't easy, he has been a constant and unwavering presence.
God is in control, TRUST, TRUST, TRUST.
Remember those you love and treat them well. The old cliche rings true-you find out who your true friends are when hard times hit. Its not an easy realization but its part of life.
If you're thinking about someone-let them know. You are not guaranteed another day.
Slow down and be---be happy--be joyful--be content--be grateful---just be.
Breathe--take a breath-appreciate it-take a deeper one and be thankful.
Don't look at someone wearing a mask like they have the bubonic plague.
Don't pretend like me having a double lung transplant is the elephant in the room--if you have questions-ask. Ask how I am, ask about the transplant, just don't pretend it didn't happen.
Just keep living until you feel alive again...after many months-I'm starting to feel alive again.
Never give up!
Live life, love life, give life!!!!!
To register to be an organ donor visit: www.organdonor.gov
Click on your state in the upper right hand corner
On my bathroom mirror
Please comment below on your thoughts/experience during the past year from YOUR view.
Saturday, October 10, 2015
Thank you Donor
This was sent off in early August, you cant give out your full name or address. I'm not sure if this will show up well, but hopefully you can enlarge to see.
Thank you for the gift of life, I pray memories are giving you some comfort as you mourn your loved one 1yr later.
Wednesday, September 9, 2015
To Whom It May Concern...
Dear person with the cough,
COVER YOUR MOUTH! I never understand how people are so inclined to share their germs. I get children have a hard time covering or may not be quick enough, but a grown adult?!?!?!
Kids are back in school, germs are shared. Cold and flu season are rapidly approaching and germs are shared. But one does have the control to: a) Stay home from work until you are over your illness, b) WEAR A MASK if you insist on strolling in public places, c) Wash your hands!
Now, I hear the rebuttal--I can't afford to stay home from work, masks are hot, I can't breathe, I don't have a fever...
Can you afford to infect your co-workers and then have to do their work while they are gone?
I assure you 100% that you CAN breathe thru those thin paper masks. And you don't have to have a fever to be contagious.
How do you think you got your current symptoms--from someone not covering a cough or a sneeze, a contaminated computer keyboard/mouse/pen/glass, talking to someone, etc.
http://www.cdc.gov/flu/about/disease/spread.htm
Yes, people stare and ask questions but once you tell them you are preventing the spread of germs, they are thankful for your proactiveness.
What is the first thing you see in many doctor offices and hospitals? COVER YOUR COUGH and they provide masks--but I've never seen anyone grab a mask. You're coughing all over and you don't think you need to contain your germs a bit??
Coughing into your elbow (not your hands) helps a bit but guess what--those tiny microscopic respiratory droplets can spread up to 9ft!
I work in a doctors office where patients want protection from other sick patients, coworkers want protection from sick patients and other coworkers, yet there is so much grumbling about wearing a mask.
Example: Adult coworker cough, cough, cough, I have a cold, my throat hurts, I have the chills.
2nd coworker: Better not let Joyce hear...
The more adequate response should be: You should wear a mask and protect others if you are going to stay here.
My bat ears hear a cough from a mile away.
I don't care if you aren't right next to me, germs travel. And you should think of protecting everyone not just me. Be an example of what is right to do.
I've worked my butt off to come back from this lung transplant and the serious complications that happened. I've worked hard everyday to get to my 60% lung function and you think its ok to not wear a mask because its uncomfortable?!?
This may be no big deal to you but a simple little virus to someone who has NO immune system can be detrimental. Hospitalization, permanent loss of lung function--the lung function that I've worked so hard to obtain- I don't have as much wiggle room with my function as some due to my complications.
Why put myself at risk working in a doctors office? I pray for protection everyday, my job is to help others-this is my calling. Am I not allowed to have some semblance of normal in my life?
A cold is no big deal to you but I have a 7 yr old that needs his mommy, I have a husband who needs his wife, I have a family that would like to see me be well and live long.
I don't enjoy the stares or questions when I wear my mask but its part of the deal. And if it means I can stay healthy then I'm doing it. I swallow 30pills a day, exercise daily, do my lung exercises daily, and am trying to stay alive. Its not a joke.
So for others around you, please cover your cough.
COVER YOUR MOUTH! I never understand how people are so inclined to share their germs. I get children have a hard time covering or may not be quick enough, but a grown adult?!?!?!
Kids are back in school, germs are shared. Cold and flu season are rapidly approaching and germs are shared. But one does have the control to: a) Stay home from work until you are over your illness, b) WEAR A MASK if you insist on strolling in public places, c) Wash your hands!
Now, I hear the rebuttal--I can't afford to stay home from work, masks are hot, I can't breathe, I don't have a fever...
Can you afford to infect your co-workers and then have to do their work while they are gone?
I assure you 100% that you CAN breathe thru those thin paper masks. And you don't have to have a fever to be contagious.
How do you think you got your current symptoms--from someone not covering a cough or a sneeze, a contaminated computer keyboard/mouse/pen/glass, talking to someone, etc.
http://www.cdc.gov/flu/about/disease/spread.htm
Yes, people stare and ask questions but once you tell them you are preventing the spread of germs, they are thankful for your proactiveness.
What is the first thing you see in many doctor offices and hospitals? COVER YOUR COUGH and they provide masks--but I've never seen anyone grab a mask. You're coughing all over and you don't think you need to contain your germs a bit??
Coughing into your elbow (not your hands) helps a bit but guess what--those tiny microscopic respiratory droplets can spread up to 9ft!
I work in a doctors office where patients want protection from other sick patients, coworkers want protection from sick patients and other coworkers, yet there is so much grumbling about wearing a mask.
Example: Adult coworker cough, cough, cough, I have a cold, my throat hurts, I have the chills.
2nd coworker: Better not let Joyce hear...
The more adequate response should be: You should wear a mask and protect others if you are going to stay here.
My bat ears hear a cough from a mile away.
I don't care if you aren't right next to me, germs travel. And you should think of protecting everyone not just me. Be an example of what is right to do.
I've worked my butt off to come back from this lung transplant and the serious complications that happened. I've worked hard everyday to get to my 60% lung function and you think its ok to not wear a mask because its uncomfortable?!?
This may be no big deal to you but a simple little virus to someone who has NO immune system can be detrimental. Hospitalization, permanent loss of lung function--the lung function that I've worked so hard to obtain- I don't have as much wiggle room with my function as some due to my complications.
Why put myself at risk working in a doctors office? I pray for protection everyday, my job is to help others-this is my calling. Am I not allowed to have some semblance of normal in my life?
A cold is no big deal to you but I have a 7 yr old that needs his mommy, I have a husband who needs his wife, I have a family that would like to see me be well and live long.
I don't enjoy the stares or questions when I wear my mask but its part of the deal. And if it means I can stay healthy then I'm doing it. I swallow 30pills a day, exercise daily, do my lung exercises daily, and am trying to stay alive. Its not a joke.
So for others around you, please cover your cough.
Sunday, August 2, 2015
The roller coaster of life called transplant
I've passed the 9mos mark since my transplant and the 1yr lungaversary is just around the corner. My 40th bday is days away (gulp) and I can't help but reminisce about this past year.
Before you are transplanted the team warns you about various probable setbacks that occur after transplant. When you hear those things, I thought those sound horrible but doable-I can't breathe anymore-what could be worse?!?! I was told by the social worker before transplant that 'everyone rejects in their first year', I still remember that and I'm just waiting for that to HIT me one day. But then I realize just because she said it doesn't mean its going to happen. She is nice and wonderful but she cannot predict the future. She doesn't hold my future in her hands.
The last 9 1/2 mos have been a major roller coaster rider with the last 2 mos more smoother. When I think back to that call that came on a beautiful sunny mild afternoon in October it makes me emotional. All my docs pre-transplant said I would do great and I believed them but I forgot they don't my future either and what happened post-op was definitely not great. Chest tubes weren't coming out or if they did my lung would collapse and I had to go back for another, my CXR on the right still looked funny. I wasn't able to get back to GR, MI as soon as I thought I would. And just when I was feeling stronger and getting semi-used to all the meds I was being pumped full of (and my eyes were back to normal after seeing squiggles on the walls and peoples pants from the huge amounts of steroids), I was told I had to go back to surgery and reopen the right side of my lung so the RLL could be removed and a muscle flap could take its place. That was devastating-I'm crying right now thinking about it. When I first saw that wound (on top of the original that stretches armpit to armpit) on the right I cried. I have a indentation where ribs were taken out and I thought I looked like a mutant. Looking at it now still upsets me.
I finally got to come home days before Thanksgiving with 2 chest tubes, somehow one fell out a week later and I ended back inpatient at the local hospital Butterworth.
I continued to battle the nasty ever changing bacteria pseudomonas--this was found on numerous bronchs during my hospital stays and I had to stay on IV antibiotics until this past Feb (4mos). I then developed a nasty colon infection that occurs from antibiotic use called c-diff early March. I haven't had a normal bowel movement since before transplant.
In June, my bronch grew out some rare fungus and worry again ensued my transplant team. We are still watching this closely but thankfully after much more testing things look stable.
You are warned pre-transplant about all these possibilities but nothing could ever prepare you. I am certain I have some post traumatic stress from my experiences from last fall-I didn't mention it up there but when you are awake with a tube down your throat it is the most AWFUL experience and I've made it clear to many around me don't ever want to be intubated again.
I could also go into the ICU psychosis that develops post op from the meds, shock to your body, and severe lack of sleep. Greg has good stories he's keeping.
The point being not only do I have a healthy fear of hair, now I am paranoid about catching any germ, bacteria, fungus, allergen, etc. I walk in anywhere and can hear the cough/sneeze 3 aisles down, 10 booths away--those with me don't hear it but its like I have Bat ears--the sonar always working.
I don't want to have acute rejection and be pumped full of high dose steroids and potentially lose the precious lung function I 'm working so hard to gain. That's the other thing--when you have 2 healthy lungs and God forbid you do have rejection and lose some you usually have something to work with. I don't have a lot of wiggle room with Charlie (my left lung) and I haven't named my remaining healthy right upper lobe. (Suggestions welcome)
So thanks to all your prayers and support currently I'm doing good besides the paranoia that I'm working on. I also want to encourage you to take care of yourselves. Do you worry about what you put in your mouth--was that vegetable cleaned? Is the meat cooked thru? That's part of my life now, it is was it is but just be aware. Also, I find it very disheartening when able bodied people don't take care of themselves. There is nothing physically wrong with you and you don't exercise because you don't want to ? Its too boring? REALLY?!!! S*@*@*#*@#*@ How lucky you are to have that choice and shame on you for not treating that body like the well oiled machine it is. I hate sweating and I've never sweated like I do now, and I can honestly say that exercising is not some great fun activity for me. I've heard all the excuses-but there is always something you can do positive for your body--can't run or walk-then bike-don't have access to a bike-do chair exercises-walk up 3 stairs a few times a day-DO SOMETHING. You don't have to agree with my opinion, that's fine. I have a responsibility to these lungs to take care of them, as well as to my family so I can be here for them.
These lungs of mine--given to me by someone's grieving family--think hard about that...it is almost an impossible concept to wrap one's mind around. Someone has died so I could benefit.
Thank you letter next on my list to my donors family, how difficult...
The roller coaster is taking off again--hang on tight!
Before you are transplanted the team warns you about various probable setbacks that occur after transplant. When you hear those things, I thought those sound horrible but doable-I can't breathe anymore-what could be worse?!?! I was told by the social worker before transplant that 'everyone rejects in their first year', I still remember that and I'm just waiting for that to HIT me one day. But then I realize just because she said it doesn't mean its going to happen. She is nice and wonderful but she cannot predict the future. She doesn't hold my future in her hands.
The last 9 1/2 mos have been a major roller coaster rider with the last 2 mos more smoother. When I think back to that call that came on a beautiful sunny mild afternoon in October it makes me emotional. All my docs pre-transplant said I would do great and I believed them but I forgot they don't my future either and what happened post-op was definitely not great. Chest tubes weren't coming out or if they did my lung would collapse and I had to go back for another, my CXR on the right still looked funny. I wasn't able to get back to GR, MI as soon as I thought I would. And just when I was feeling stronger and getting semi-used to all the meds I was being pumped full of (and my eyes were back to normal after seeing squiggles on the walls and peoples pants from the huge amounts of steroids), I was told I had to go back to surgery and reopen the right side of my lung so the RLL could be removed and a muscle flap could take its place. That was devastating-I'm crying right now thinking about it. When I first saw that wound (on top of the original that stretches armpit to armpit) on the right I cried. I have a indentation where ribs were taken out and I thought I looked like a mutant. Looking at it now still upsets me.
I finally got to come home days before Thanksgiving with 2 chest tubes, somehow one fell out a week later and I ended back inpatient at the local hospital Butterworth.
I continued to battle the nasty ever changing bacteria pseudomonas--this was found on numerous bronchs during my hospital stays and I had to stay on IV antibiotics until this past Feb (4mos). I then developed a nasty colon infection that occurs from antibiotic use called c-diff early March. I haven't had a normal bowel movement since before transplant.
In June, my bronch grew out some rare fungus and worry again ensued my transplant team. We are still watching this closely but thankfully after much more testing things look stable.
You are warned pre-transplant about all these possibilities but nothing could ever prepare you. I am certain I have some post traumatic stress from my experiences from last fall-I didn't mention it up there but when you are awake with a tube down your throat it is the most AWFUL experience and I've made it clear to many around me don't ever want to be intubated again.
I could also go into the ICU psychosis that develops post op from the meds, shock to your body, and severe lack of sleep. Greg has good stories he's keeping.
The point being not only do I have a healthy fear of hair, now I am paranoid about catching any germ, bacteria, fungus, allergen, etc. I walk in anywhere and can hear the cough/sneeze 3 aisles down, 10 booths away--those with me don't hear it but its like I have Bat ears--the sonar always working.
I don't want to have acute rejection and be pumped full of high dose steroids and potentially lose the precious lung function I 'm working so hard to gain. That's the other thing--when you have 2 healthy lungs and God forbid you do have rejection and lose some you usually have something to work with. I don't have a lot of wiggle room with Charlie (my left lung) and I haven't named my remaining healthy right upper lobe. (Suggestions welcome)
So thanks to all your prayers and support currently I'm doing good besides the paranoia that I'm working on. I also want to encourage you to take care of yourselves. Do you worry about what you put in your mouth--was that vegetable cleaned? Is the meat cooked thru? That's part of my life now, it is was it is but just be aware. Also, I find it very disheartening when able bodied people don't take care of themselves. There is nothing physically wrong with you and you don't exercise because you don't want to ? Its too boring? REALLY?!!! S*@*@*#*@#*@ How lucky you are to have that choice and shame on you for not treating that body like the well oiled machine it is. I hate sweating and I've never sweated like I do now, and I can honestly say that exercising is not some great fun activity for me. I've heard all the excuses-but there is always something you can do positive for your body--can't run or walk-then bike-don't have access to a bike-do chair exercises-walk up 3 stairs a few times a day-DO SOMETHING. You don't have to agree with my opinion, that's fine. I have a responsibility to these lungs to take care of them, as well as to my family so I can be here for them.
These lungs of mine--given to me by someone's grieving family--think hard about that...it is almost an impossible concept to wrap one's mind around. Someone has died so I could benefit.
Thank you letter next on my list to my donors family, how difficult...
The roller coaster is taking off again--hang on tight!
Subscribe to:
Posts (Atom)